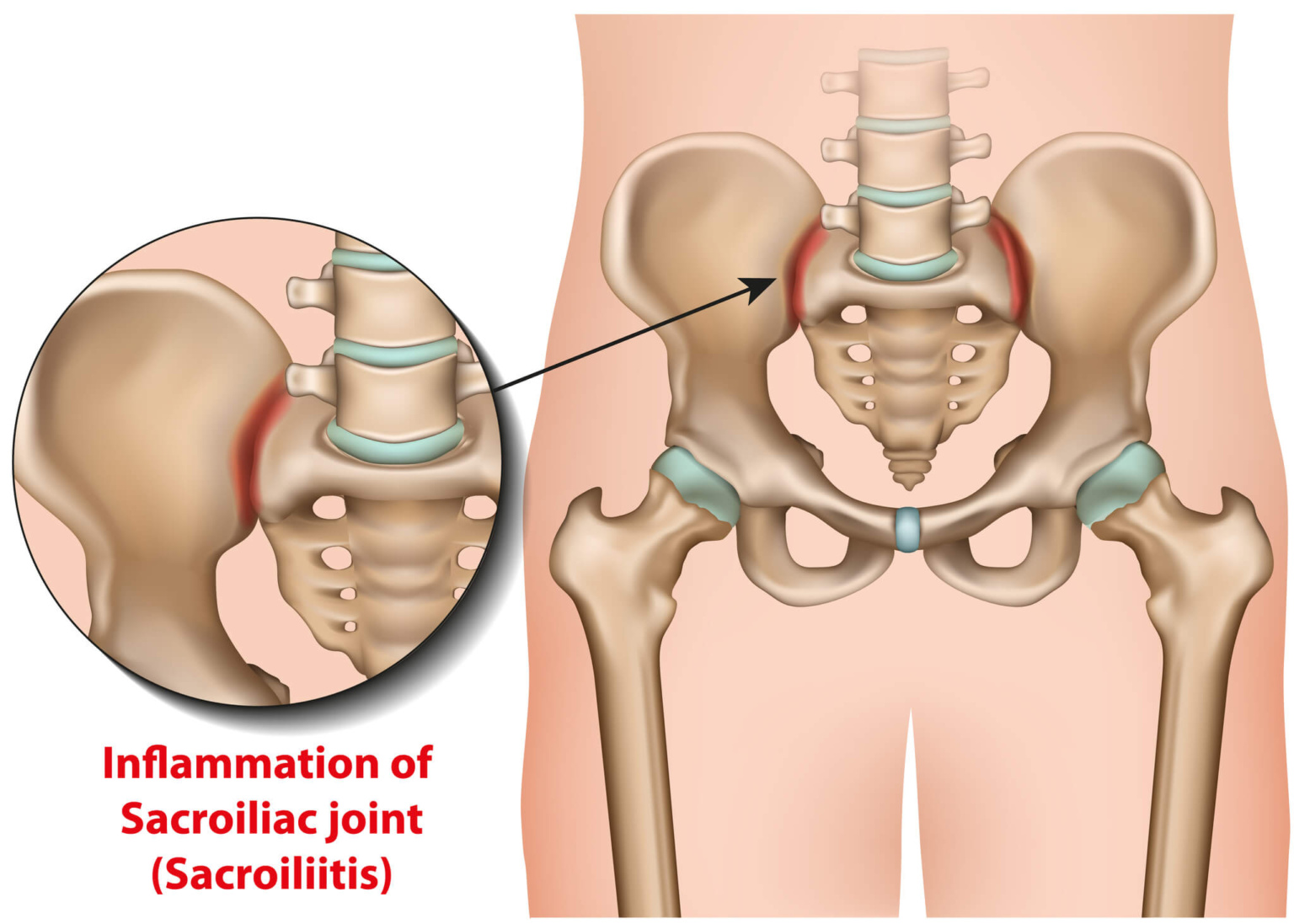
Sacroiliitis is a painful condition that affects the sacroiliac joints located near the lower spine and pelvis. This inflammation can lead to significant discomfort in the buttocks and lower back, often radiating down one or both legs (not to be confused with sciatica). Activities that involve prolonged standing, sitting, or movements such as climbing stairs can exacerbate the pain, making everyday tasks particularly difficult.
Due to its symptoms overlapping with other types of lower back pain, sacroiliitis is frequently misdiagnosed, complicating the patient’s journey to relief. Additionally, it is associated with a spectrum of diseases known as spondyloarthropathies, which are types of inflammatory arthritis affecting the spine, such as undifferentiated spondyloarthropathy, reactive arthritis, reiter’s syndrome, psoriatic arthritis, and others. Effective treatment of sacroiliac joint pain and sacroiliitis typically combines physical therapy with medication to manage pain and reduce inflammation, aiming to improve quality of life for those affected by this condition.
In this blog, we will dive deeper into the causes of sacroiliitis, explore how it is diagnosed, and discuss comprehensive treatment options to help manage this debilitating condition.
Is Sacroiliitis the Same as Sacroiliac Joint Pain?
Sacroiliitis and sacroiliac joint pain are related but somewhat distinct, and it’s important to understand the differences between them for accurate diagnosis and effective treatment.
Sacroiliac joint pain refers to any discomfort or pain in the sacroiliac joint area, which could be due to various reasons such as mechanical issues, overuse, or even pregnancy. This type of pain is generally felt in the lower back and buttocks and may radiate to the surrounding areas. The causes of sacroiliac joint pain can range from physical activity that strains the joint, misalignment, or degeneration over time.
Sacroiliitis, on the other hand, specifically involves inflammation of one or both of the sacroiliac joints. Unlike broader sacroiliac joint pain, sacroiliitis is diagnosed by a healthcare provider through clinical evaluation, symptoms assessment, and sometimes imaging tests. The inflammation associated with sacroiliitis can cause pain, which may be similar to other forms of lower back pain but is distinct in its origin.
Essentially, sacroiliitis always involves sacroiliac joint pain, but just because you have sacroiliac joint pain doesn’t mean that you’re suffering from sacroiliitis.
Symptoms of Sacroiliitis
- Persistent Lower Back Pain: The hallmark of sacroiliitis is pain in the lower back. This discomfort can vary in nature:
- Position-Related Aggravation: The pain typically intensifies after prolonged periods of sitting or standing in one position. Changing positions frequently can help alleviate the discomfort temporarily.
- Movement Sensitivity: Pain often worsens when rotating or turning the hips, making activities that involve twisting movements particularly painful.
- Variable Intensity: The pain may feel sharp and stabbing at times, or it could be a more constant, dull ache depending on the activity and time of day.
- Radiating Pain: The pain can spread from the lower back into adjacent areas such as the buttocks, hips, or thighs. This radiating pain can affect one or both sides of the body, complicating movements like walking or climbing stairs.
- Morning Stiffness: Many individuals experience significant stiffness first thing in the morning. While it’s normal to feel some stiffness after sleeping or sitting, the stiffness caused by sacroiliitis usually persists for more than an hour after waking up.
- Increased Discomfort with Certain Activities: Activities that can exacerbate sacroiliitis symptoms include:
- Sleeping or sitting for extended periods.
- Standing for long durations.
- Uneven weight distribution on the legs.
- Stair climbing and running.
- Taking large steps.
Causes of Sacroiliitis
Sacroiliac joint pain and sacroiliitis can arise from a variety of factors. Here’s a list of the primary causes:
- Injury: Trauma from motor vehicle accidents or falls can directly damage the sacroiliac joints.
- Osteoarthritis: Known as wear-and-tear arthritis, it degrades joint cartilage, causing stiffness and pain.
- Ankylosing Spondylitis: This form of arthritis affects the spine and can significantly inflame the sacroiliac joints.
- Pregnancy: Hormonal changes during pregnancy loosen the sacroiliac joints, while increased weight and altered gait add stress.
- Infection: Rare but serious, infections like those caused by Staphylococcus aureus can lead to sacroiliitis.
- Psoriatic Arthritis: Combines the joint inflammation of arthritis with the skin symptoms of psoriasis.
- Gastrointestinal Diseases: Inflammatory conditions like Crohn’s disease and ulcerative colitis can cause sacroiliitis.
- Reactive Arthritis and Behçet’s Disease: These inflammatory diseases can also affect the sacroiliac joints.
Diagnosis
Diagnosing sacroiliitis involves physical examinations, imaging tests, and possibly blood tests to accurately assess the condition and its underlying causes. Here’s how healthcare providers typically diagnose sacroiliitis:
Physical Examination
During the initial consultation, your healthcare provider will conduct a thorough examination of your back, hips, and legs. You will be asked about the onset of your symptoms, activities that exacerbate the pain, and any other health conditions you might have. This information helps in understanding the potential causes and nature of your sacroiliitis.
The physical exam may include:
- Range of Motion Tests: Your provider might have you perform movements to assess the range of motion in your hips and legs. This helps identify any limitations or pain triggered by specific positions.
- Palpation: Pressing on various areas around the sacroiliac joints to identify tender spots or pain triggers.
- Stress Tests: Gently moving your legs into different positions to stress the sacroiliac joints and pinpoint the source of pain.
Imaging Tests
Imaging tests are crucial for visualising the bones and tissues of the sacroiliac joints and surrounding areas. These may include:
- Pelvis X-rays: Can reveal signs of damage or changes in the sacroiliac joints.
- Computed Tomography (CT) Scan: Provides a more detailed image, useful for diagnosing sacroiliitis and assessing the extent of joint damage.
- Magnetic Resonance Imaging (MRI): Especially effective in detecting sacroiliitis early, particularly if ankylosing spondylitis is suspected. MRI can show soft tissue and bone inflammation not visible on X-rays.
Additional Diagnostic Tests
In some cases, further testing may be required:
- Blood Tests: These can help rule out infections or other inflammatory conditions that might cause symptoms similar to sacroiliitis.
- Numbing Shots: Injecting numbing medication directly into the sacroiliac joint. If the pain significantly diminishes following the injection, it likely confirms that the sacroiliac joint is the pain source.
These diagnostic tools and methods allow healthcare providers to accurately diagnose sacroiliitis and tailor a treatment plan that addresses the specific needs and conditions of the patient. Early and precise diagnosis is key to effectively managing and treating sacroiliitis, helping patients return to a more active and pain-free life.
Treatment
Treating sacroiliitis involves tailoring a plan to the individual’s specific symptoms and the underlying causes of the condition. Here’s an overview of the common and specialised treatment options available:
Physical Therapy
Physical therapy is often the cornerstone of treatment for sacroiliitis, focusing on:
- Strengthening Exercises: These exercises help strengthen the muscles around the sacroiliac joints, reducing pressure on the joints and enhancing stability.
- Range of Motion Exercises: These are designed to increase flexibility and mobility in the sacroiliac joints, helping to alleviate stiffness and pain.
Contact us today to find out more about how we can help you treat your sacroiliac joint pain.
Medications
Various medications are used to manage pain and inflammation associated with sacroiliitis:
- NSAIDs: Over-the-counter nonsteroidal anti-inflammatory drugs, such as ibuprofen and naproxen, are commonly used to reduce inflammation and alleviate pain. It’s important to use these under the guidance of a healthcare provider due to potential long-term side effects.
- Muscle Relaxers: Prescription medications like cyclobenzaprine may be used to ease muscle spasms associated with sacroiliitis.
- Corticosteroids: These can be injected directly into the affected joint to provide significant pain relief and reduce inflammation.
- Biologics: For autoimmune-related sacroiliitis, biologic medications, including TNF inhibitors and IL-17 inhibitors, help control immune system responses that contribute to inflammation.
- DMARDs: Disease-modifying antirheumatic drugs, especially JAK inhibitors, are another option for reducing inflammation.
Advanced Treatments
When conventional treatments do not provide adequate relief, more advanced procedures may be considered:
- Radiofrequency Ablation (RFA): This procedure uses radiofrequency energy to disable nerve fibres carrying pain signals to the brain, providing long-term pain relief.
- Electrical Stimulation: Implanting an electrical stimulator in the lower spine can help reduce pain by interrupting pain signals.
- Joint Injections: Corticosteroid injections into the joint can reduce swelling and pain, although their use is generally limited to a few times a year to avoid potential side effects on bones and tendons.
Surgery
Surgery for sacroiliitis is rare but may be recommended if other treatments have failed to improve symptoms:
- Joint Fusion: In severe cases, surgery might involve fusing the bones of the sacroiliac joint together with surgical screws to alleviate pain by stabilising the joint.
Specialist Consultation
Working with a specialist, such as a rheumatologist, is often beneficial, especially for those whose sacroiliitis is linked to an inflammatory disease. These specialists can provide targeted treatments that address the specific autoimmune or inflammatory conditions contributing to sacroiliitis.
How to Prevent Sacroiliitis
Prevention is always better than treatment! While there is no real prevention for sacroiliitis, if you have any of the risk factors such as arthritis, ankylosing spondylitis, psoriatic arthritis, inflammatory bowel diseases (including Crohn’s disease and ulcerative colitis), you should at least try the following:
Avoid Tobacco Products: Smoking and the use of other tobacco products can exacerbate inflammation and increase the risk of various arthritic conditions.
Engage in Low-Impact Exercise: Activities such as swimming, cycling, or walking can help maintain joint flexibility and muscle strength without placing excessive strain on the joints.
Maintain a Healthy Diet and Exercise Routine: Following a balanced diet and keeping an active lifestyle are crucial for overall joint health and can help manage weight, reducing stress on the joints.
Choose Benchmark Physio
If you live in the Sydney area and suffer from sacroiliitis, contact us today. We have years of experience in managing and treating various joint and musculoskeletal conditions, and our team of expert physiotherapists is dedicated to providing personalised care that addresses your specific needs. We employ a comprehensive approach that includes the latest treatment techniques and a focus on holistic well-being to ensure you achieve the best possible outcomes. Start your journey towards recovery and regain the quality of life you deserve.